1241
Views & Citations241
Likes & Shares
An unnatural communication between the maxillary
sinus and oral cavity is known as oroantral communication (OAC). If this
communication fails to close spontaneously, it gets epithelialized to form an
oroantral fistula (OAF). The most common cause of an OAC/OAF is the extraction
of a maxillary molar or premolar. However, sometimes ill-placed implants
without adequate knowledge or radiographic assistance can lead to OAF
formation.
Keywords: Complication
of implant placement, Maxillary sinus, Oroantral communication, Oroantral
fistula
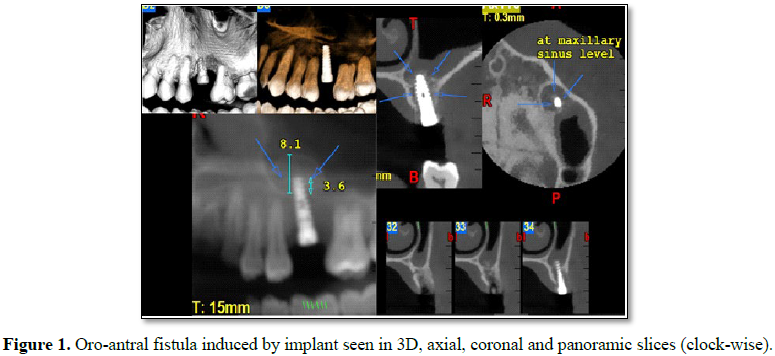
CLINICAL IMAGE
A 45 year old male patient was referred for a
Cone beam computed tomography (CBCT) view post an implant placement. CBCT of
field of view 5*5 was taken, which revealed implant placed in region of 26
going at least 1 cm beyond the level of apices of adjacent teeth suggestive of
breaching the floor of the maxillary sinus. 3-dimensional views, panoramic view
and sectional views confirmed the breach thus suggestive of an oro-antral
fistula induced because of improper implant placement (Figure 1). Measurement revealed that the implant was about 3.6 cm
beyond the floor of the maxillary sinus. The patient was referred back to the
dentist for removal of implant and imminently required closure of the fistula.
The patient can present with variable
immediate or delayed symptoms. The reason for a delayed response is because the
closure of the communication due to blot clot or implant as in this case. OACs
must be treated as soon as possible to avoid sinus conditions, which can
prevent the treatment of the lesion and the resolution of the case. Most
importantly, the infection must be resolved before any surgical procedure for
OAC closure is undertaken and sinus irrigation along with systemic antibiotic
therapy should be administered. In the case of small perforations of the sinus,
when there are no signs of sinusitis, spontaneous healing is possible, while in
the case of larger perforations, the chance of spontaneous healing is less [2].
Closing this communication is important to
avoid food and saliva contamination that could lead to bacterial infection,
impaired healing, chronic sinusitis and such various complications [3].
Numerous surgical methods have been described for the treatment of OAFs
although only a few have been accepted in daily practice. Some of the commonest
techniques include: Buccal Flap, Palatal Flap, Modified Palatal Flap and
Pedicled Buccal Fat Pad graft. Furthermore, at times the use of a combination
technique such as a BFP with a buccal advancement flap can give more stability
than using any conventional method alone [4].
1.
Ozkan A, Durmaz C
(2015) Alternative surgical management of oro-antral fistula using auricular
cartilage. J Clin Exp Dent 7: e339-e341.
2.
Filho V, Giovanella F,
Karsburg RM, Torriani MA (2010) Oroantral communication closure using a
pedicled buccal fat pad graft. Rev Odonto Ciênc 25: 100-103.
3.
Borgonovo AE,
Berardinelli FV, Favale M, Maiorana C (2012) Surgical options in oro-antral
fistula treatment. Open Dent J 6: 94-98.
4.
Pauly G, Kashyap RR,
Shetty R, Kini R, Rao PK, et al. (2017) Oro-antral fistula: Radio-diagnostic
lessons from a rare case. J Diagn Imaging 2: 21-24.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)